Clinical characteristics and antimicrobial therapy of healthcare-associated carbapenem-non-susceptible gram-negative bacterial meningitis: a 16-year retrospective cohort study | BMC Infectious Diseases

Bacterial isolates and antimicrobial susceptibility
From January 1, 2004 to December 31, 2019, 912 non-duplicate CSF isolates were collected from adult inpatients. Of these, 407 (44.6%) were Gram-positive cocci and 505 (55.4%) were Gram-negative bacilli. Among the Gram-negative bacilli isolates, 423 (83.8%) were collected from post-surgical patients.
The predominant seven groups of bacilli accounted for 87.9% (444/505) of Gram-negative isolates: A. baumannii complex (35.4%, 179/505), K. pneumoniae (25.0%, 126/505), Pseudomonas aeruginosa (9.5%, 48/505), Escherichia coli (5.7%, 29/505), A. lwoffii (5.1%, 26/505), Stenotrophomonas maltophilia (4.6%, 23/505), and Enterobacter cloacae (2.6%, 13/505). Other Enterobacterales included K. aerogenes (n = 6), Proteus mirabilis (n = 5), K. oxytoca (n = 4), Serratia marcescens (n = 4), and others (n = 4). Other non-fermentative bacteria included other Pseudomonas species (n = 5), Chryseobacterium indologenes (n = 6), A. junii (n = 5), Comamonas testosteroni (n = 4), Elizabethkingia meningoseptica (n = 3), Brevundimonas diminuta (n = 3), and others (n = 7). During the 16-year period, A. baumannii complex remained the most common isolate, while the number of K. pneumoniae isolates showed an increasing trend (Fig. 2).

Distribution of Gram-negative bacteria isolated from the central nervous fluid of adult inpatients with healthcare-associated meningitis from 2004 to 2019 (n = 505). A Proportion of Acinetobacter baumannii complex, other non-fermentative bacteria, Klebsiella pneumoniae, other Enterobacterales, and other species isolated from the CSF per year. B Trend of the proportion of Acinetobacter baumannii complex and Klebsiella pneumoniae isolated from the CSF per year
Of the 505 Gram-negative isolates, 122 strains did not resuscitate; thus, antimicrobial susceptibility testing with the broth dilution method was performed in 383 strains (Table 1). The resistance rates of Acinetobacter spp. (n = 170) to imipenem and meropenem were as high as 50.0% and 50.6%, respectively. For Klebsiella spp. (n = 106), the resistance rates to imipenem and meropenem were 43.4% and 42.5%, respectively. During 2004 and 2013, a markedly increasing trend of the resistance to carbapenems was observed in both Acinetobacter spp. and Klebsiella spp., while the resistance rate fluctuated around 58.3–92.9% and 40.0–88.2% during 2014 and 2019, respectively (Fig. 3).
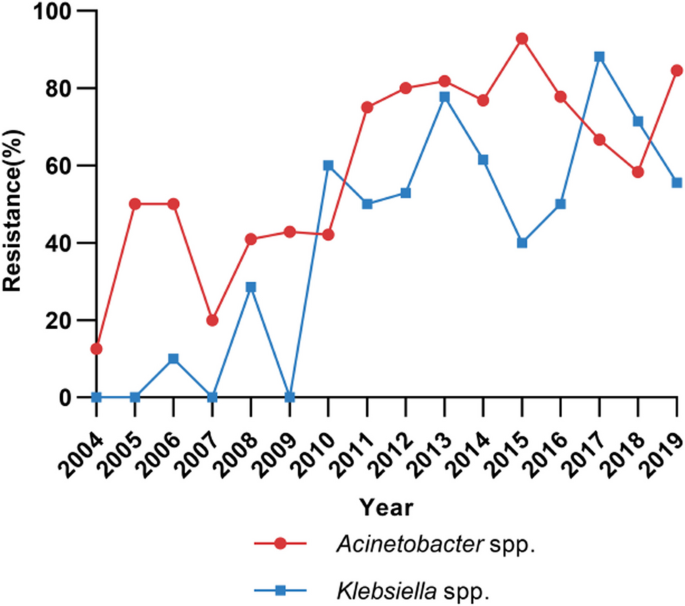
Trends of meropenem-resistance rates in Acinetobacter spp. (n = 170) and Klebsiella spp. (n = 106) isolated from cerebrospinal fluid
Clinical characteristics and risk factors of Carba-NS Gram-negative bacterial meningitis
Since the hospital information system only started reserving electronic data in 2016, the archives of some patients hospitalized before 2016 had information missing (n = 181). Therefore, a total of 324 cases were included for analysis of clinical characteristics. All of the 324 isolates collected from these patients had antimicrobial susceptibility testing reports from the Clinical Microbiology Department of the hospital, of which 299 were resuscitated and had MIC testing. The distribution of pathogens in these cases was as follows: (1) Enterobacterales (n = 124): K. pneumoniae (n = 89), E. coli (n = 15), E. cloacae (n = 4), K. aerogenes (n = 4), S. marcescens (n = 4), P. mirabilis (n = 3), and others (n = 5); (2) A. baumannii complex (n = 124); and (3) other Gram-negative bacteria (n = 76): P. aeruginosa (n = 27), S. maltophilia (n = 16), A. lwoffii (n = 13), C. indologenes (n = 4), A. junii (n = 4), E. meningoseptica (n = 3), and others (n = 9).
The clinical characteristics of the 308 patients with healthcare-associated Gram-negative bacterial meningitis (excluding 16 cases caused by S. maltophilia, which are intrinsically resistant to carbapenems) and comparison between the Carba-NS Gram-negative bacterial meningitis group (n = 186) vs. the Carba-S Gram-negative bacterial meningitis group (n = 122) are presented in Table 2. Most patients in both groups had an intensive care unit (ICU) stay, received neurosurgical procedures and general anesthesia, presented with fever, and showed increased white blood cell (WBC) and neutrophil counts in blood. Both groups of patients had increased levels of WBCs and multinuclear cells and decreased chloride and glucose in the CSF.
Compared to the Carba-S group, the Carba-NS group had a higher proportion of male patients (73.1% vs. 59.0%; P = 0.010), with older age (median age 50.0 vs. 44.5; P = 0.020), and lower GCS score (P < 0.001). The diagnosis was more frequently related to cerebrovascular disease (38.7% vs. 27.0%; P = 0.035) and traumatic brain injury (37.6% vs. 21.3%; P = 0.002) but was less common in intracranial tumors (16.7% vs. 42.6%; P < 0.001). Patients in the Carba-NS group also had more non-CNS infections, such as pneumonia, sepsis, and urinary tract infection on admission (37.1% vs. 16.4%; P < 0.001), as well as hospitalization in the previous month (67.2% vs. 50.5%; P = 0.003).
During hospitalization, the Carba-NS group patients more frequently received mechanical ventilation (52.7% vs. 33.6%; P = 0.001), intra-cranial pressure (ICP) monitor (23.7% vs. 9.8%; P = 0.002), Ommaya (51.1% vs. 37.7%; P = 0.021), with a higher rate of carbapenems exposure (44.1% vs. 30.3%; P = 0.015) but a lower proportion of administration of glucocorticoids (38.7% vs. 55.7%; P = 0.003), proton pump inhibitor (PPI) use (67.2% vs. 80.3%; P = 0.012), ventriculoperitoneal (VP) shunt (11.8% vs. 23.8%; P = 0.006), and continuous lumbar drainage (52.2% vs. 65.6%; P = 0.020), compared to the Carba-S group. On the first day of infection, patients in the Carba-NS group more frequently suffered from serum hypoalbuminemia (62.6% vs. 48.0%; P = 0.020), and the levels of protein in the CSF were higher (5315.0 ± 377.0 mg/L vs. 4074.5 ± 511.3 mg/L; P = 0.048) compared to those in the Carba-S group.
Carba-NS group patients have a higher in-hospital mortality rate than Carba-S group patients (18.8% vs. 7.4%; P = 0.005). Kaplan–Meier survival analysis also revealed that the rate of in-hospital mortality was significantly higher among patients infected with Carba-NS Gram-negative bacilli than those infected with Carba-S bacilli (P = 0.001). Moreover, the mortality rate among the A. baumannii meningitis group was significantly higher than that among the K. pneumoniae group and other Gram-negative bacterial groups (P < 0.001) (Fig. 4A and B).
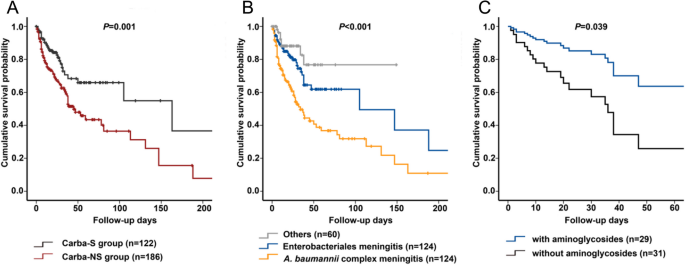
Survival analysis of patients with Gram-negative bacterial meningitis from 2004 to 2019. A Kaplan–Meier survival analysis of patients infected with Carba-NS Gram-negative bacterial meningitis compared to patients infected with Carba-S Gram-negative bacterial meningitis (P = 0.001). B Kaplan–Meier survival analysis of patients infected with Acinetobacter baumannii complex meningitis compared to patients infected with Enterobacterales meningitis and other Gram-negative bacterial meningitis (P < 0.001). C Cox survival analysis for the use of aminoglycosides for Carba-NS Enterobacterales meningitis (P = 0.039)
Univariate analysis revealed that male sex, age, GCS score, cerebrovascular disease, traumatic brain injury, with non-CNS infection on admission, hospitalization in the month before admission, mechanical ventilation, carbapenems exposure, ICP monitor, and Ommaya were significantly associated with Carba-NS Gram-negative bacterial meningitis, whereas intracranial tumor, patients with glucocorticoids or PPI, VP shunt, and continuous lumbar drainage were associated with Carba-S Gram-negative bacterial meningitis. Multivariate analysis of these factors showed that independent risk factors associated with Carba-NS Gram-negative bacterial meningitis included severe coma (GCS 3–8) (odds ratio [OR]: 2.935; 95% CI: 1.675–5.143; P < 0.001), non-CNS infections on admission (OR: 2.690; 95% CI: 1.459–4.960; P = 0.002), application of ICP monitoring (OR: 2.237; 95% CI: 1.052–4.755; P = 0.036), and carbapenems exposure (OR: 2.019; 95% CI: 1.195–3.413; P = 0.009) (Table 2).
Antimicrobial treatment and clinical outcomes of Carba-NS Gram-negative bacterial meningitis
Cases with detailed medical records of treatment and outcomes were collected. Except for S. maltophilia meningitis cases, the clinical success rate of the Carba-NS group (49.5%, 92/186) was lower than that of the Carba-S group (57.4%, 70/122), without statistical significance (P = 0.174). Enterobacterales and A. baumannii complex were two of the most common pathogens of Carba-NS meningitis.
Carba-NS enterobacterales meningitis
Of the 124 cases of Enterobacterales meningitis, the clinical success rate of the Carba-NS group (51.6%, 32/62) was lower than that of the Carba-S group (67.7%, 42/62), with no statistical significance (P = 0.067). Among 62 patients with Carba-NS Enterobacterales meningitis, 60 (96.8%) patients received therapy involving active agents, with an efficacy rate of 53.3% (32/60), while two (3.2%) patients received therapy without active agents, and both cases failed to respond to treatment. The clinical efficacy rates of patients who received monotherapies and combination therapies were both 53.3% (8/15 vs. 24/45). Comparing the 2004–2009 group with the 2010–2019 group, the clinical efficacy rates (61.9% [13/21] vs. 59.2% [61/103]) showed no significant differences (P = 0.819).
For the 60 cases of Carba-NS Enterobacterales meningitis with active agents, the clinical efficacy rate of the aminoglycoside-based (including amikacin [n = 21, administered as 0.8 g q24h ivgtt], gentamicin [n = 4], isepamicin [n = 4]) combination therapy group (69.0%, 20/29) was higher than that of the non-aminoglycosides therapy group (38.7%, 12/31, P = 0.019). Among the 29 cases in the aminoglycoside-based therapy group, 23 received aminoglycosides by intravenous injection alone, 3 received aminoglycosides by both intravenous and intrathecal/intraventricular routes, and 3 received aminoglycosides by the intrathecal/intraventricular route alone. Carbapenems (administered as meropenem 2 g q8h ivgtt with prolonged infusion for 2–3 h) were the most commonly used antimicrobial agent in aminoglycoside-based combination therapy (75.9%, 22/29), and the clinical efficacy rate of the carbapenem-aminoglycoside-based group (68.2%, 15/22) was higher than that of the carbapenem-based group (without aminoglycosides) (22.2%, 4/18, P = 0.004). Moreover, the clinical efficacy rate of the SXT (two tablets, oral, twice a day, with 400 mg of SMX and 80 mg of TMP per tablet)-based therapy group (81.8%, 9/11) was higher than that of the non-SXT therapy group (46.9%, 23/49, P = 0.036) (Table 3). The clinical efficacy of regimens with fosfomycin (58.8%, 10/17) vs. regimens without fosfomycin (51.2%, 22/43) showed no significance (P = 0.592).
Additionally, multivariate analysis showed that the use of aminoglycosides was associated with improved efficacy (OR: 3.519; 95% CI: 1.209–10.24; P = 0.021) (see Additional file 1). Cox regression showed that the use of aminoglycosides was an independent factor for survival (hazard ratio [HR]: 0.371; 95% CI: 0.144–0.952; P = 0.039) (Fig. 4C). However, Cox regression showed that SXT was not significantly associated with survival (HR: 0.028; 95% CI: 0.000–1.610; P = 0.084) (see Additional file 2).
Carba-NS A. Baumannii complex meningitis
For the 124 cases of A. baumannii complex meningitis, the clinical success rate was not statistically significant between the Carba-NS group (45.1%, 41/91) and Carba-S group (51.5%, 17/33; P = 0.524). These patients were commonly afflicted by A. baumannii complex pneumonia and bloodstream infections; 51 (56.0%) and 8 (8.8%) cases for the Carba-NS group, respectively, and for the Carba-S group, 16 (48.5%) cases were co-infected with A. baumannii complex pneumonia. Among the 91 patients with Carba-NS A. baumannii complex meningitis, 82 (90.1%) received therapy involving active agents. All nine patients who received inappropriate therapy without active agents failed to respond to the treatment. The clinical efficacy rates of patients who received monotherapies (41.7%, 5/12) and combination therapies (51.4%, 36/70) showed no statistical significance (P = 0.532). Comparing the 2004–2009 group with the 2010–2019 group, the clinical efficacy rates (45.2% [19/42] vs. 47.6% [39/82]) did not show significant differences (P = 0.806).
For the 82 cases of Carba-NS A. baumannii complex meningitis with active agents, the clinical efficacy rate of the tetracycline-based (including tigecycline [n = 21, the first dosage was 100 mg, followed by 50 mg q12h ivgtt], doxycycline [n = 12], and minocycline [n = 2]) therapy group (62.9%, 22/35) was higher than that of the non-tetracycline therapy group (40.4%, 19/47, P = 0.044) (Table 3). Multivariate analysis indicated that tetracyclines were associated with efficacy improvement (OR: 2.494; 95% CI: 1.014–6.132; P = 0.047) (see Additional file 3). Cox regression showed that the use of tetracyclines was not an independent factor for survival (HR: 0.930; 95% CI: 0.501–1.726; P = 0.817).
The clinical efficacy rates were not statistically significant between the sulbactam-based (administered as cefoperazone 2.0 g plus sulbactam 1.0 g q8h ivgtt) therapy group (52.5%, 21/40) and the non-sulbactam therapy group (47.6%, 20/42; P = 0.659). Meanwhile, the clinical efficacy rates of the carbapenem-based group, sulbactam-based group, and carbapenem-sulbactam-based group were 37.9% (11/29), 56.5% (13/23), and 47.1% (8/17), respectively. No statistical significance was observed among these three groups (P = 0.409).
S. maltophilia meningitis
Analysis of 16 S. maltophilia cases showed that the clinical success rate was 68.8% (11/16) and the in-hospital mortality rate was 12.5% (2/16). Levofloxacin, SXT, and tetracyclines were the most commonly used antibacterial agents. No statistical significance was observed among the different therapy groups.
link